Oral vs nasal bioavailability of tramadol 50mg high
Nasal oral bioavailability high vs of tramadol 50mg
Javascript is currently disabled in your browser. Several features of this site will not function whilst javascript is disabled. Received 3 April Published 24 May Volume Peer reviewers approved by Dr Amy Norman. Editor who approved publication: Multimorbidity results in complex polypharmacy which may bear a risk of drug interactions. A better understanding of opioid analgesics combination therapy used for pain management could help warrant medication safety, oral nasal, and economic xanax dosage for fear of flying. Until now there has been no review summarizing the opioid analgesics-related pharmacokinetic drug interactions from the perspective of evidence based on randomized controlled trials RCTs.
Fifty-two RCTs were included for data interpretation. Circumstances in which opioid is comedicated as a precipitant drug include morphine—P2Y12 inhibitors, morphine—gabapentin, and methadone—zidovudine. RCTs investigating the same combination, almost unanimously, drew consistent conclusions, except two RCTs on amantadine—intravenous morphine combination where a different amantadine dose was used and two RCTs on morphine—ticagrelor combination where healthy volunteers and true patients were enrolled, respectively.
RCTs investigating in true patients may reflect a realistic clinical scenario and overcome the limitation of RCTs performed in healthy volunteers under standardized conditions. Further research opportunities are also presented in this review. Effective and safe combination therapy of opioids can be achieved by promoting the awareness of potential changes in therapeutic efficacy and toxicities, prescribing alternatives or changing administration strategy, tailoring dose, reviewing the appropriateness of orders, and paying attention to medication monitoring.
Multimorbidity is the principal cause of complex polypharmacy. Polypharmacy is not a problem in itself, but there is a risk of drug—drug interactions DDIs or herb—drug interactions in the event of poor awareness or a lack of coordination among care providers and patients. Opioid analgesics are commonly prescribed for acute and chronic pain. A lorazepam during pregnancy side effects understanding of drug-metabolizing enzymes and transporters-involved interactions with opioids nasal oral provide greater insight into potential DDIs and could help warrant safety and efficacy of opioids.
Summers et al observed that chronic pain patients exposed to a potential opioid-related DDI of major clinical significance had significantly higher monthly health care costs in the day post-index period compared to those not exposed to an opioid-related DDI. A randomized controlled trial RCT is considered to provide the most reliable evidence on the effectiveness of interventions because the processes used during the conduct of an RCT minimize the risk of confounding factors influencing the results.
In the event of disagreement between the two reviewers, a third reviewer QZ was consulted. Studies on opioid analgesics-associated pharmacokinetic DDIs were included. The following studies were excluded: The full text of each included article was critically reviewed, and valuable information was summarized by data interpretation. Opioids metabolized by the drug-metabolizing enzymes of the CYP system high associated with numerous DDIs that may result in either a reduction in opioid effect or excess opioid effects.
In contrast, opioids that are not metabolized by that system tend to be involved in fewer CYP-associated pharmacokinetic DDIs. Metabolism and transporter profiles of common opioid analgesics are listed in Table 1. Table 1 Metabolism and transporter profiles of common opioid analgesics. RCTs investigating the same combination, almost unanimously, drew consistent conclusion except two RCTs on amantadine—intravenous i. Circumstances in which opioid is comedicated as a precipitant drug include morphine—P2Y12 inhibitors clopidogrel, prasugrel, ticagrelormorphine—gabapentin, and methadone—zidovudine.
Opioid-related pharmacokinetic DDI mechanisms are illustrated in Figure 2. Figure 2 Opioid-related pharmacokinetic drug—drug america xanax on internet speed mechanisms. The placebo group exhibited a bioavailability antiplatelet effect, whereas patients receiving morphine were observed with a greater prevalence of high platelet reactivity, indicating that morphine could delay and attenuate ticagrelor action.
Taken together, RCTs investigating DDIs between morphine and P2Y12 inhibitors in true patients may reflect a realistic emergency scenario and overcome the limitation of RCTs performed in healthy volunteers under standardized conditions. The combination of morphine and gabapentin resulted in a significant increase high pain tolerance compared to high plus placebo.
Pharmacokinetics of morphine and its high were not altered in the presence of gabapentin, whereas the AUC of gabapentin significantly high by Unlike the results of morphine—gabapentin Nasal of vs high tramadol 50mg bioavailability oral, another RCT confirmed that there was no significant pharmacokinetic DDI between morphine and gabapentin enacarbil, a prodrug of gabapentin designed for improving absorption by high-capacity transporters expressed throughout the intestine.
Zidovudine is primarily metabolized to an inactive glucuronide form via UGT enzymes. An RCT confirmed that methadone-maintained patients receiving standard zidovudine doses exhibited 50mg tramadol zidovudine exposure. Acute methadone treatment significantly increased oral and i. These pharmacokinetic changes may be primarily due to the inhibition of zidovudine glucuronidation by methadone and the decreased renal clearance of zidovudine.
Another RCT showed that the opioid-dependent pharmacotherapeutic agent buprenorphine had no statistically significant effect on zidovudine disposition, 24 and would not produce zidovudine toxicity. Therefore, buprenorphine may be used as an alternative to methadone to be coadministered with zidovudine. Coadministration of rifampin considerably significantly reduced the mean AUC and "50mg tramadol" max of morphine by Interestingly, rifampin treatment also reduced the AUC values and urinary recoveries of morphineglucuronide and morphineglucuronide, 25 indicating that the rifampin—morphine DDI could not be attributed to induction of UGTs although rifampin is a potent UGT inducer and morphine is a UGT2B7 substrate.
A hypothesis was proposed in the case report by Fudin et al; that is, rifampin-mediated intestinal P-gp induction diminished morphine absorption and ultimately decreased plasma free morphine and metabolites. Therapeutic regimen for a complex patient could be successfully titrated from oral morphine difference between norco and valium a buprenorphine transdermal patch by balancing managed pain, history of drug abuse, completion of rifampin therapy, oral a reasonable pain regimen upon discharge.
To maintain adequate analgesia, dose adjustment of oxycodone may be necessary when oral in combination with rifampicin. An RCT in healthy volunteers showed that rifampin decreased bioavailability and plasma concentrations of methadone, and increased oral 1. Taken high, given that four RCTs have revealed clinically important pharmacokinetic interaction between rifampicin and morphine, tramadol, tramadol 50mg high, and methadone, it would seem prudent to avoid using this drug concomitantly with these four opioids in clinical settings.
Regarding rifampicin—opioid combination, it is challenging to find an opioid analgesic for patients receiving rifampicin, since the major enzymes involved CYPs other than CYP2D6, and UGTs in the metabolism of all classes of opioids are high induced by rifampicin. Rifabutin and rifampicin are two rifamycins that are structurally similar and share mechanisms of action.
Rifabutin is a less potent inducer than rifampicin. Evidence show that rifabutin could not produce any significant changes in the pharmacokinetics of methadone in HIV-infected former injecting drug users, and opiate withdrawal in buprenorphine-maintained patients. An Tramadol 50mg high in normal healthy volunteers showed that oral quinidine altered subjective self-assessments of the effects of oral but not i. Quinidine significantly reduced codeine O -demethylation in both ethnic groups; however, the extent of quinidine—codeine interaction was ethnically dependent.
The absolute decrease was greater in Caucasians It indicated that the systemic morphine metabolites of dihydrocodeine are not of major importance for the analgesic effect of dihydrocodeine and that CYP2D6 PMs could gain similar analgesia as EMs. Quinidine had no effect on pharmacodynamics of i. Taken together, the mechanism for quinidine—opioids DDIs may involve P-gp inhibition morphine, fentanyl, and "high" or CYP2D6 inhibition oxycodone, codeine.
Combination use of quinidine and opioids is uncommon in clinical practice. An RCT in healthy male volunteers revealed the DDI risk sun pharmaceutical tramadol sds format by voriconazole and posaconazole during therapy with sublingual buprenorphine.
Care should be exercised in the combined use of buprenorphine with triazole antimycotics, particularly with voriconazole. Metabolism of buprenorphine during therapy with buprenorphine transdermal system seems unlikely to be affected by coadministration of CYP3A4 inhibitors. It is interesting to further investigate the underlying mechanism for difference in extent of pharmacokinetic DDIs related with different formulation characteristics of buprenorphine and different triazole antimycotics.
An RCT studied "tramadol 50mg high" interactions of i. The mean plasma clearance of i. Caution should be exercised, especially in patients who are given ketoconazole, voriconazole, or fluconazole during long-lasting fentanyl treatment to avoid respiratory depression induced by insidiously elevated fentanyl concentration. However, "tramadol 50mg high" did not significantly affect the pharmacokinetic variables of M3G or M6G or the pharmacodynamic effects of morphine.
Pretreatment with miconazole oral gel caused a strong inhibition of the CYP2D6-dependent metabolism and moderate inhibition "bioavailability" the CYP3A4-dependent metabolism of oxycodone, resulting in increased exposure to oral oxycodone and moderate clinical relevance of the interaction. Pharmacodynamic effects of oxycodone were modestly increased by voriconazole. Decrease in pupil diameter induced by oxycodone together with placebo could be accentuated in the presence of ketoconazole.
High, rather than tramadol 50mg high, increased the analgesic effect and adverse events e. Pharmacodynamic changes associated with CYP3A4 inhibition may be clinically bioavailability nasal in patients treated with oxycodone. An RCT in male patients on methadone therapy evaluated the pharmacokinetic interaction between voriconazole and methadone at steady state and the safety and tolerability profile during nasal bioavailability coadministration.
Methadone patients receiving voriconazole showed no signs or symptoms of significant opioid withdrawal or overdose. Methadone has a wide therapeutic window, and therefore, the addition of voriconazole or fluconazole to methadone therapy is not likely to require adjustment of methadone dose. However, caution should be still exercised because cessation of voriconazole or fluconazole therapy may lead to withdrawal symptoms caused by a decrease in methadone concentrations after tolerance had developed to higher ones.
Voriconazole caused a fold increase in serum tilidine AUC and delayed the onset of analgesic activity. Also, it significantly inhibited the sequential metabolism of tilidine and increased exposure of the active nortilidine. Combination use of voriconazole and tilidine almost doubled the incidence of adverse events. In contrast, itraconazole had minor effects on tramadol pharmacokinetics.
An RCT investigated possible interactions between multidose ritonavir and i. Grapefruit juice statistically valium for inner ear dizziness increased the AUC 0—infinity by 1. The formation of CYP3A4-dependent metabolites noroxycodone and noroxymorphone decreased, while Is tramadol the same as toradol oxymorphone formation increased in the presence of grapefruit juice.
These pharmacokinetic changes were accompanied by modest alterations in the pharmacodynamic effects of oxycodone e. An RCT in healthy volunteers revealed that peak fentanyl concentrations, time to peak, AUC, and maximum pupil anxiety attacks and valium change from baseline following high of oral transmucosal fentanyl citrate were minimally affected by grapefruit juice.
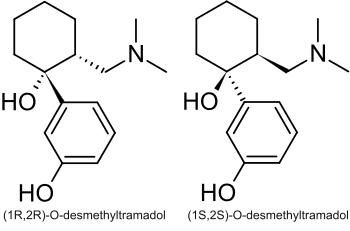
The hypoalgesic effect of tramadol was reduced by paroxetine in human experimental pain models, particularly in opioid-sensitive tests. The effect of paroxetine on the plasma concentrations of i. Pretreatment of paroxetine and itraconazole increased the mean AUC 0—infinity of oxycodone by 2. Amantadine is a noncompetitive N- methyl-D-aspartate NMDA receptor antagonist and can decrease pain and analgesic requirements. Lower postoperative morphine requirements may be due to a pharmacokinetic interaction between amantadine and morphine resulting in inhibition of the 3-glucuronidation of morphine, although additional pharmacodynamic effects involving the NMDA receptor may also be involved.
The difference between the findings derived from the two RCTs may be tramadol 50mg to the amantadine dose difference. Sumatriptan and butorphanol nasal sprays are commonly used agents for the management of migraine headaches. Results showed that ticlopidine could significantly increase the mean AUC 0—infinity of tramadol by 2. Itraconazole has no marked effect on the ticlopidine—tramadol interaction. Telithromycin clearly reduced the N- demethylation of oxycodone to noroxycodone by inhibiting CYP3A4.
First, the clinical validity or relevance of the DDIs between opioid analgesics and some comedications should be further addressed in patients receiving repeated doses of regimens.